Obsessive Compulsive Disorder (OCD) is a complex mental health condition that may be understood as a neurological difference or form of neurodivergence[1]. About 1-2% of people live with OCD. It is common for people to experience a persistent unwanted thought or to have particular routines. However, the diagnosis of OCD is made only when there is significant mental distress and/or considerable disruption and dysfunction in everyday life[2]. OCD is often first experienced as a child or adolescent, and can disrupt a student’s ability to attend school, to participate in classroom activities, and to engage with learning. While diagnosis and treatment is the province of clinicians[3], school staff play a vital role in creating an environment where the student feels supported to challenge OCD and pursue their educational goals[4].
What are obsessions and compulsions?
Our creative minds are constantly active, and some of the ideas, images, and urges that we come up with are both unexpected and unwelcome. It is an everyday occurrence to have intrusive thoughts that are fleeting and soon forgotten[5]. For example, students might wonder if an animal has peed on the ground they are about to sit on, or whether they really did put homework in their schoolbag. They might see an image of putting out a leg and tripping up a passer-by, or they might feel an impulse to jump off a high place. Generally students may feel a slight discomfort but do not feel a need to respond to such thoughts, and the thoughts are confirmed as meaningless when nothing dreadful happens.
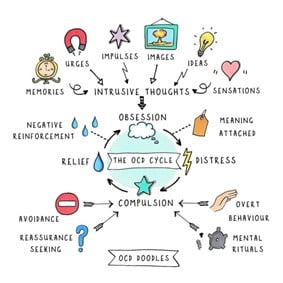
Image from OCD Doodles reproduced with permission.
By contrast, as the above graphic illustrates, a person caught up in the obsessive-compulsive cycle worries that certain intrusive thoughts are meaningful. The individual wonders whether there might be a real threat, and whether the disturbing thought might say something about them as a person. For example, the thought that I might not have remembered to wash my hands might mean that my best friend will get ill and even die, and that I might be a danger to others. Naturally a train of thought like this will be associated with uncomfortable emotions such as anxiety, fear, disgust, and shame. Sometimes, rather than a conscious thought, a student may simply have a nagging sensation that something does not feel right, and this can seem unbearable.
Compulsive behaviours are an attempt to neutralise the emotional distress associated with intrusive thoughts. These may be physical actions such as checking, handwashing, or lining things up a certain number of times or ways. Compulsions can also be mental rituals such as silently repeating a mantra or continually going over memories of an incident. An individual may be driven to repeat again and again an action such as tying a shoelace until a ‘just-right’ sensation is achieved. Common behaviours that are not always recognised as being compulsions are repeatedly seeking reassurance from other people such as teachers, friends, and parents, and avoiding feared situations.
Engaging in a compulsion provides temporary relief from the emotional distress associated with an intrusive thought. However, carrying out a compulsion also strengthens the person’s belief that the intrusive thought is meaningful and that they need to avoid having it, or to seek escape from such thoughts and associated emotions. In the longer term, reacting to intrusive thoughts as though they are meaningful results in further unwanted thoughts of a similar nature and so, once drawn into the obsessive-compulsive cycle, intrusive thoughts may return again and again, and the individual may become very distressed.
The unwanted repetitive thoughts are called obsessions, and are often concentrated around a particular theme such as a fear of harm to self or others, contamination, or being a morally bad person. It is important to understand that obsessive thoughts are egodystonic – they are disturbing because they go against the person’s values and sense of identity. The individual feels doubt or fear, rather than an intention or desire.
The neuroscience of OCD
There are complex genetic factors that predispose some people to develop OCD[6]. In identical twins, if one twin has OCD then there is about a 50% chance that the other twin will also have OCD. Life events also play a role. OCD may develop following a trauma[7], and symptoms may worsen at times of stress such as illness or during exams. Certain beliefs and thinking patterns are common in people who experience OCD, such as inflated responsibility and threat estimation, believing that having a thought makes an event more likely to happen, black-and-white thinking, an intolerance of uncertainty, and/or perfectionism[8].
Neurobiological research suggests that OCD may involve a ‘brain glitch’ in communication between the orbitofrontal cortex and the basal ganglia[9]. In broad terms, the orbitofrontal cortex, which is located at the front of the brain about the eye sockets, is active when the brain detects something dangerous or potentially threatening. A message is sent from the orbitofrontal cortex to the basal ganglia, an area of the brain which is involved in movement, including goal-directed actions, habitual responses, and switching to new behaviours. The basal ganglia both initiates a response to the danger or potential threat and sends inhibitory feedback to the orbitofrontal cortex. It is thought that in OCD there may be an imbalance between the activation and inhibitory pathways in this communication loop, such that the individual gets stuck and keeps repeating a behaviour rather than having a sense of completion and being able to move on.
Medications that affect the activity of neurotransmitters such as serotonin are helpful for some people who experience OCD. Currently this is a trial-and-error process, as it is not yet possible to predict which medication at what dosage may be helpful for a particular individual[10].
OCD was traditionally grouped in clinical classification systems with anxiety disorders such as generalised anxiety, phobia, and post-traumatic stress. As understanding has evolved, a separate group for obsessive-compulsive related disorders has been created, encompassing hoarding disorder, skin picking and hair pulling, body dysmorphic disorder, and also health anxiety[11]. It is common for someone to be diagnosed with several of these conditions. Consistent with the view that OCD is a form of neurodivergence, someone who is autistic or has ADHD and/or tics, such as Tourette syndrome, is more likely to also have OCD (and vice-versa)[12].
The role of cognitive behavioural therapy in OCD treatment
The meaning that is attached to unwanted thoughts and emotions changes how an individual feels about and reacts to them. A therapist with expertise in cognitive behavioural therapy, and in particular in OCD treatment, will begin by providing psychoeducation about the obsessive-compulsive cycle. A core component of OCD treatment is Exposure Response Prevention therapy, in which the individual gradually learns to tolerate the occurrence of intrusive thoughts and uncomfortable emotions, and to refrain from carrying out any compulsive behaviours. As well as ‘moving away’ from listening to OCD, an important motivation is to ‘move towards’ the individual’s true values and goals[13].
Because OCD has a neurobiological component and is not an illness to be cured, an individual needs to come to terms with a brain that may be constantly trying to ‘alarm’ them. A degree of separation between their core sense of self and the experience of OCD is necessary: in other words, you are not your thoughts. It can be helpful to give the OCD ‘voice’ a name, and to use a metaphor such as a bully, a crank caller, or a friend who is trying to be helpful but is not.
OCD and school engagement
School is often a setting in which issues related to OCD manifest, and it may even be a teacher who first notices unusual behaviour or that a student seems distressed. OCD should be viewed not simply as a health matter to be handled by health professionals, but also as a psychological disability that can seriously interfere with a student’s wellbeing and engagement in school. For example, see this personal account of how unrecognised OCD profoundly affected one New Zealand student’s experience of school.
In a Canadian study, researchers surveyed parents on the impacts of OCD on their child’s school experience. Many parents reported a negative impact of OCD on their child’s ability to function at school. For example, students would avoid attending specific classes, talking to specific people, using the school bathroom, and/or eating at school. There were difficulties in completing homework or spending excessive time to complete homework, in social interaction, and indeed in attending school at all. Most parents disclosed their child’s diagnosis to the school, but others did not because of concerns such as the possibility of their child being treated badly by their peers, and the fear that their child’s information would become permanent in the school records. Parents who did disclose considered that this improved things or effected no change, but rarely made things worse[14].
To date, in New Zealand there seems to have been little research on the educational experience of learners with psychological disability during primary and secondary school. In 2022, the Education Review Office together with the Human Rights Commission and the Office for Disability Issues reported on how well the New Zealand education system is supporting disabled learners in mainstream schools. However, the focus was on learners with physical, intellectual, cognitive, and sensory impairments, and forms of neurodivergence such as dyslexia, Development Coordination Disorder, and autism. There was unfortunately no specific consideration of psychological disability[15].
New Zealand parents sometimes mention that their child’s OCD has become so severe that they are no longer able to regularly attend the local school. Some students with OCD attend regional health schools as part of their treatment plan, and some parents decide that their child needs to be home-schooled. Annually there are over 1,000 enrolments at the national correspondence school Te Kura via the psychological/psychosocial gateway[16], and among these will be an unknown number of students with OCD (moreover, if students are over the age of 16, then no justification is needed for enrolment of a student with Te Kura).
OCD and educational attainment
Unsurprisingly, OCD can have a considerable impact not only on a child’s experience of school but also on their educational attainment. Individual lived-experience accounts are beginning to be backed up by international research studies looking at whether students continued with their education and how they performed in examinations. There is currently a lack of local research on the educational attainment of students with OCD but, in Denmark, a nationwide study of students born between 1988 and 1999 found that 79% of female and 69% of male students with OCD took the final examination of compulsory schooling, compared with 91% and 86% of those without a mental disorder[17]. These findings suggest that some students dropped away from their schooling. A study from Sweden which looked at people who were born between 1976 and 1998 found that individuals with OCD were significantly less likely to have passed courses at the end of compulsory school, and to have finished upper secondary school, started a university degree, and finished postgraduate education, although this study cohort may have been weighted towards individuals with more severe OCD symptoms[18].
OCD in the classroom
There are many ways that OCD can affect students at school[19]. It may highly visible or completely invisible to others, but it is important to remember that, either way, it usually causes embarrassment and shame. While each student is unique and so is their experience of OCD, the following examples illustrate some of the ways that OCD might manifest in school settings.
A student getting ready for school may worry that they have not packed the right items, which leads them to check their backpack’s contents repeatedly and consequently arrive late for school. While at school, they may worry about coming into contact with contaminated objects, leading to an avoidance of touching shared objects such as worksheets being passed along or communal art materials. Some obsessions may be focused on schoolwork, such as ensuring their handwriting is ‘just right’, or worrying that they have misunderstood something they need to read. These thoughts may lead them to repeat their work over and over in search of an elusive level of perfection, work very slowly, or be hesitant to answer questions or engage with the teacher over their work.
Other intrusive thoughts may be unrelated to the school setting, such as a fear that something bad will happen to a parent or loved one, leading them to constantly repeat a prayer or mantra and consequently fail to pay attention to what is happening in class. They may worry that they have inadvertently done something bad like lying, cheating, or making someone ill, which leads them to constantly seek reassurance from others, or apologise for things they have not done.
How teachers and schools can support students with OCD
It is a natural reaction for an anxious child to ask others to become involved in their compulsive behaviours. For example, it is common to seek reassurance from an adult: Did I wash my hands enough? Did I do something bad? Have I done this schoolwork right? Teachers can help by both validating the experience (this feels really scary for you) and expressing confidence that the student is strong enough to manage OCD[20].It is legitimate to provide accurate and realistic information, but unhelpful to engage in conversation with OCD by repeatedly going over the same ground, as this simply feeds the obsessive-compulsive cycle. Bear in mind that attempting to achieve absolute certainty leads to doubt rather than confidence. OCD is not logical and does not play fair – it is inconsistent and frequently changes targets. Expect that a student will have good and bad days, but look for progress over the longer term.
When OCD symptoms are troublesome, the purpose of any accommodations is to support the student to continue to engage in education. But the longer-term goal is to improve management of OCD so that accommodations can be phased out. A student who is wrestling with OCD is strengthened by things that they enjoy and are good at, and a student who is struggling to complete work during class has all the more need of their break time. Participating in a therapy session or tackling an exposure task can be utterly exhausting, and a teacher should give some room for a student to recover from this work. Be sure to celebrate effort and any wins, however small.
There should also be regular communication between the school, family, and clinical team so that everyone is on board with respect to current treatment goals, and to ensure that any problems can be addressed as they arise. Bear in mind, though, that parents whose child has been newly diagnosed with OCD reportedly often find themselves placed in the position of trying to explain OCD to school staff, despite being themselves at the beginning of their journey in learning about OCD and how to support their child.
Another important consideration is listening to and consulting the students themselves. For example, students involved in a Canadian qualitative study exploring youth perspectives made a number of recommendations regarding how schools could support students with OCD, which included meaningful education for school staff about OCD, confidential and personalised supports, and the ability for students to identify the areas where they needed support rather than receiving blanket provision. They also recommended that teachers engage in active listening and intermittent checking to gain a better understanding of students’ personalised needs[21].
Families and schools can work together to create a safer and more informed space for students (and for school staff and parents) who experience OCD by sharing positive examples of people experiencing and in recovery from OCD. For example, the Kiwi singer-songwriter Benee and the Harry Potter actor Daniel Radcliffe have talked openly about seeking support for OCD. A silver lining to experiencing OCD is a strengthening of resilience, empathy, and self-knowledge.
Similarly there are now books for children and young people which feature characters with OCD. For instance, The Thunderbolt Pony by Stacy Gregg concerns the adventures of a twelve-year-old girl with OCD in the aftermath of the Kaikoura earthquake. The picture book Mr Worry: A Story about OCD by Holly Niner follows a young boy as he develops OCD symptoms, is diagnosed, and learns how to ignore unwanted thoughts. This book provides insight into how OCD might manifest in the home and classroom.
To help talk to children about the nature of thoughts, the picture book Just a Thought by children’s author and psychotherapist Jason Gruhl is an exploration of the thoughts generated by our weird, wacky and wonderful minds. In some cases, it may not be until adulthood that an individual discloses their unwanted distressing thoughts and discovers that they have been living with unrecognised OCD, even though they first experienced them in childhood or adolescence. Therefore, having conversations about the nature of thoughts will help all students understand that not all thoughts should be treated as meaningful, and that having an unwanted scary or embarrassing thought does not make you a bad person.
Language matters
People in the OCD community generally do not use identity-first language for OCD. Thus someone is not an obsessive-compulsive student, but rather a student who has, experiences, or lives with OCD. While common, it is not appropriate to describe someone as ‘a little OCD’ because they are tidy, meticulous, or passionate about something they enjoy. Such usages perpetuate misconceptions and stereotypes about actual OCD. True clinical OCD is far beyond what people joke about when they say they have OCD. It is an experience of mental distress with symptoms waxing and waning in severity, and can be debilitating. Because OCD is often first experienced as a child or adolescent, it is particularly important that school staff have an awareness and understanding of the condition and how to support a student who is experiencing OCD.
Recommended resources and further reading
In New Zealand, people living with OCD or supporting someone living with OCD can seek help from a Facebook-based community called Fixate, and from a local OCD-specific website. Parents and teachers of children diagnosed with OCD can find links to international sources of information about OCD, and also to related conditions such as body dysmorphic disorder, on this website.
Of particular value is the Anxiety in the Classroom website created by USA-based organisation the International OCD Foundation. Some of the information on this website is based on OCD: A Handbook for School Personnel, a book by Gail Adams published in 2011, which provides information about how OCD affects students and has practical advice for educational professionals. Also useful is a concise, practical handout from a Canadian organisation called Identifying and supporting students with OCD in schools.
More recently, clinical researcher Professor Eli Lebowitz has developed the Supportive Parenting for Anxious Childhood Emotions (SPACE) programme, which focuses on the responses of the parent rather than on their child with anxiety and/or OCD. The insights and advice arising from his work are also pertinent to classroom teachers seeking to understand and support a student with anxiety and/or OCD. The book Breaking Free of Child Anxiety and OCD explains the reasoning behind the SPACE approach and gives step-by-step advice on its implementation.
Finally, an episode from the Attitude series features a New Zealand family in which two sisters live with OCD, tics, and depression. This is a great way to gain insight into what it means to live with and manage OCD.
Many thanks to Laura Johnson of OCD Doodles for permission to reproduce her doodle.
Endnotes
[1] Love, S. (2022, March 30). What does it mean to have a ‘weird’ brain in the age of neurodiversity?
[2] Obsessive compulsive disorder | Mental Health Foundation
[3] BPAC NZ (2022, July 8). Recognising and managing OCD in primary care.
[4] International OCD Foundation. Anxiety in the classroom;
Negreiros, J. (n.d.) Identifying and supporting students with OCD in schools. Anxiety Canada.
[5] Elders, A., & Tse, Y. (2022, August 17). Improving outcomes for people with obsessive-compulsive disorder. New Zealand Doctor.
[6] Goodman, W. K., Storch, E.A., & Sheth, S. A. (2021). Harmonizing the neurobiology and treatment of Obsessive-Compulsive Disorder. American Journal of Psychiatry, 178(1),17-29. doi: 10.1176/appi.ajp.2020.20111601. PMID: 33384007; PMCID: PMC8091795.
[7] Migala, J. (2023, July 10). Can childhood trauma cause OCD? NOCD.
[8] Cervin, M., McNeel, M. M., Wilhelm, S., McGuire, J. F., Murphy, T. K., Small, B. J., Geller, D. A., & Storch, E. A. (2022). Cognitive beliefs across the symptom dimensions of pediatric Obsessive-Compulsive Disorder: Type of symptom matters. Behavior Therapy, 53(2), 240-254, https://doi.org/10.1016/j.beth.2021.08.001.
[9] Goodman, Storch, & Sheth, 2021;
Graybiel, A. M., & Rauch, S. L. (2000). Toward a neurobiology of Obsessive-Compulsive Disorder. Neuron, 28(2), 343-347.
Know your brain: Obsessive-compulsive disorder. Neuroscientifically Challenged.
[10] International OCD Foundation (n.d.). About medications for pediatric OCD.
[11] OCD UK (n.d.). Diagnostic and Statistical Manual of Mental Disorders and OCD;
OCD UK (n.d.). International Classification of Diseases (ICD) and OCD.
[12] Olivardia, R. (2023, October 11). When OCD and ADHD coexist: Symptom presentation, diagnosis, and treatment. ADDitude;
Yuhas, D. (2019, February 27). Untangling the ties between autism and obsessive-compulsive disorder. Spectrum;
Katz, T. C., Bui, T. H., Worhach, J., Bogut, G., & Tomczak, K. K. (2022). Tourettic OCD: Current understanding and treatment challenges of a unique endophenotype. Frontiers in Psychiatry, 13. doi: 10.3389/fpsyt.2022.929526. PMID: 35966462; PMCID: PMC9363583
[13] The OCD Stories (2019, June 23). Dr Lisa Coyne – ACT and ERP (for children and adolescents);
Mental Health Foundation (n.d.). Review of Stuff That’s Loud: A teen’s guide to unspiralling when OCD gets noisy.
[14] Negreiros, J., Best, J.R., Vallani, T., et al. (2023). Obsessive-Compulsive Disorder (OCD) in the school: Parental experiences regarding impacts and disclosure. Journal of Child and Family Studies, 32, 2848–2857. https://doi.org/10.1007/s10826-022-02350-w
[15] Education Review Office (2022). Thriving at school? Education for disabled learners. Wellington: ERO.
[16] Education Review Office (2021, November 5). Te Aho o Te Kura Pounamu.
[17] Dalsgaard, S., McGrath, J., Østergaard, S. D., Wray, N. R., Pedersen, C. B., Mortensen, P. B., & Petersen, L. (202). Association of mental disorder in childhood and adolescence with subsequent educational achievement. JAMA Psychiatry, 77(8),797-805. doi: 10.1001/jamapsychiatry.2020.0217. PMID: 32211833; PMCID: PMC7097843.
[18] Pérez-Vigil, A., et al. (2018). Association of Obsessive-Compulsive Disorder with objective indicators of educational attainment: A nationwide register-based sibling control study. JAMA Psychiatry, 75(1), 47-55. doi: 10.1001/jamapsychiatry.2017.3523. PMID: 29141084; PMCID: PMC5833536.
[19] International OCD Foundation. Anxiety in the classroom;
Negreiros, J. (n.d.) Identifying and supporting students with OCD in schools. Anxiety Canada;
AT Parenting Survival (n.d.). OCD and anxiety in school: The most misunderstood students.
[20] Lebowitz, E. (2022). Rethinking treatment for child anxiety and OCD. TEDx.
[21] Vallani, T. I., Naqqash, Z., Lin, B., Lu, C., Austin, J. C., & Stewart, S. E. (2023). The journey from concealment to disclosure of an obsessive-compulsive disorder diagnosis in the high school setting: A qualitative study exploring youth perspectives. Psychiatry Research, 326, 115275, ISSN 0165-1781, https://doi.org/10.1016/j.psychres.2023.115275.